At Southern Maryland Foot & Ankle, we see many patients managing diabetes who are at risk of developing serious foot conditions. One of the most common complications for individuals with diabetes is the development of diabetic foot ulcers. These open sores can lead to severe infections if left untreated, making it essential to understand how to prevent, recognize, and treat them. In this blog post, we’ll discuss what diabetic foot ulcers are, their symptoms, and how we can help you manage and treat them.
What Are Diabetic Foot Ulcers?
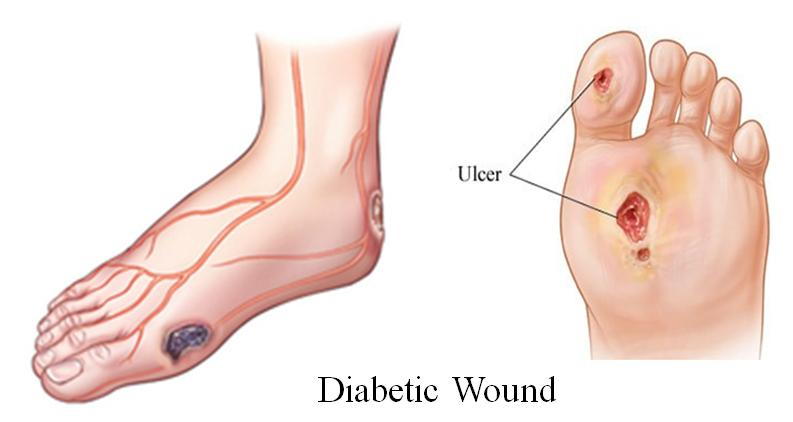
A diabetic foot ulcer is an open sore or wound that typically forms on the bottom of the foot. These ulcers are common in people with diabetes, especially those who have poor circulation, neuropathy (nerve damage), or difficulty managing their blood sugar levels. Foot ulcers can range from small, superficial wounds to deep sores that affect deeper layers of skin, muscle, and even bone.
Due to the reduced sensation in the feet caused by diabetic neuropathy, individuals with diabetes may not feel the ulcer developing. This lack of sensation, combined with poor circulation, can delay healing and make the ulcer more susceptible to infection.
Causes of Diabetic Foot Ulcers
Several factors contribute to the development of diabetic foot ulcers, including:
- Peripheral Neuropathy: Many people with diabetes experience nerve damage, particularly in the feet. This can lead to a loss of sensation, making it difficult to detect blisters, cuts, or sores.
- Poor Circulation: Diabetes can cause narrowing and hardening of blood vessels, reducing blood flow to the feet. Poor circulation can delay wound healing and increase the risk of ulcers.
- High Blood Sugar Levels: Elevated blood sugar weakens the immune system and impairs the body’s ability to heal wounds, making it easier for ulcers to form and become infected.
- Foot Deformities: Conditions like hammertoes, bunions, or calluses can create pressure points on the foot, increasing the risk of skin breakdown and ulcers.
- Improper Footwear: Wearing ill-fitting shoes can lead to blisters and sores, which may develop into ulcers if not properly cared for.
Symptoms of Diabetic Foot Ulcers
Diabetic foot ulcers may not cause pain, especially in those with diabetic neuropathy, making it essential to regularly inspect your feet for signs of a problem. Common symptoms include:
- An open sore or wound on the foot, often located on the ball of the foot or under the big toe.
- Swelling, redness, or discoloration around the ulcer.
- Drainage of pus or clear fluid from the wound, which may stain your socks or shoes.
- Foul odor coming from the ulcer, which could indicate infection.
- Thickened or callused skin surrounding the ulcer.
If the ulcer becomes infected, you may notice increased swelling, warmth, and redness, as well as fever or chills in more severe cases. Infections that go untreated can lead to complications like osteomyelitis (bone infection) or, in extreme cases, amputation.
Preventing Diabetic Foot Ulcers
Preventing foot ulcers is critical for people with diabetes. With proper care, many foot complications can be avoided. Here are some essential prevention tips:
1. Daily Foot Inspections
Make it a habit to inspect your feet daily for any signs of sores, cuts, blisters, or redness. Use a mirror or ask for help if you have difficulty seeing the bottom of your feet.
2. Wear Proper Footwear
Wearing shoes that fit well and offer adequate support is crucial. Avoid shoes that are too tight, have rough seams, or cause friction. If needed, consider custom orthotics to ensure even weight distribution.
3. Maintain Good Blood Sugar Control
Keeping your blood sugar levels within the target range helps reduce the risk of complications, including nerve damage and poor circulation, both of which contribute to foot ulcers.
4. Moisturize Your Feet
Dry skin is more prone to cracking and infections, so make sure to keep your feet moisturized. However, avoid applying lotion between your toes, as this can create a moist environment where infections can thrive.
5. Trim Toenails Carefully
Cut your toenails straight across to avoid ingrown toenails, which can lead to infection. If you have trouble trimming your nails, consider seeing a podiatrist for regular nail care.
6. Stop Smoking
Smoking can further impair circulation, delaying wound healing. If you smoke, quitting can significantly improve your overall health and reduce your risk of foot ulcers.
Diagnosing Diabetic Foot Ulcers
If you suspect you have a foot ulcer, it’s essential to seek medical attention as soon as possible. At Southern Maryland Foot & Ankle, we will:
- Examine your foot to assess the size, depth, and severity of the ulcer.
- Evaluate circulation and nerve function to determine whether poor blood flow or neuropathy is contributing to the ulcer.
- Order imaging tests, such as X-rays, if we suspect that the ulcer has affected deeper tissues or if there are signs of infection in the bone.
Treatment for Diabetic Foot Ulcers
Effective treatment for diabetic foot ulcers focuses on promoting healing, preventing infection, and managing any underlying conditions that may have contributed to the ulcer’s development. Treatment options include:
1. Wound Care
Proper wound care is essential to promote healing. This includes cleaning the ulcer regularly, applying dressings, and protecting the wound from further trauma. Our podiatry team will guide you through the best wound care practices for your condition.
2. Debridement
Removing dead or infected tissue around the ulcer (a procedure known as debridement) can help promote healing and prevent further complications. This process also allows healthy tissue to form more effectively.
3. Offloading
Reducing pressure on the ulcer, a technique called offloading, is critical for healing. Depending on the location and severity of the ulcer, you may need to wear special shoes, braces, or casts to take the pressure off the affected area.
4. Antibiotics
If the ulcer is infected, antibiotics may be prescribed to treat the infection and prevent it from spreading.
5. Improving Circulation
For patients with poor circulation, improving blood flow to the feet is essential for healing. This may involve lifestyle changes, medications, or even surgery in severe cases.
6. Surgical Intervention
In cases where the ulcer does not heal with conservative treatment or when there are complications like infection spreading to the bone, surgical intervention may be necessary. This could involve removing infected tissue or performing procedures to improve circulation.
Preventing Recurrence
Once a foot ulcer heals, preventing recurrence is vital. You can reduce the risk of developing another ulcer by following the same preventive measures mentioned earlier and scheduling regular check-ups with your podiatrist to monitor foot health.
Conclusion
Diabetic foot ulcers are a serious complication of diabetes, but with proper care and prompt treatment, they can be managed effectively. At Southern Maryland Foot & Ankle, we specialize in treating diabetic foot conditions and helping patients maintain healthy feet. If you are living with diabetes and are concerned about your foot health, don’t hesitate to reach out to us.