Infections are a very common condition in the general population and a routine cause that brings patients to our practice. Infections can be bacterial, viral, parasitic, or fungal in nature, but in this blog post, we will focus on bacteria.
Causes of bacterial infections
Direct source: if you have a cut, scrape, injury, or open blister on your foot, bacteria can enter your skin and lead to an infection.
Hematological source: if you have an infection elsewhere in your body, it can sometimes enter your bloodstream and spread to the foot.
Signs/symptoms of infection
- Foot feels warm to the touch
- Foot appears discolored, with redness, red streaks, or white patches
- Fever, chills, nausea, vomiting (associated with other signs of infection on your foot)
- Foot is swollen or fluctuant
- There is fluid or pus draining from your foot
Common bacterial infections
Erythrasma
A superficial infection of the skin caused by the bacteria, Corynebacterium minutissimum. This typically presents as macerated, scaly plaques between the toes or erythematous to brown patches or thin plaques in intertriginous areas. This can often look similar to other conditions that affect the web spaces such as tinea pedis (athlete’s foot), eczema, and dermatitis. We can often differentiate between these conditions using a Wood’s lamp which will show a coral-red fluorescence when under light. Treatment typically includes topical antibacterial medications.
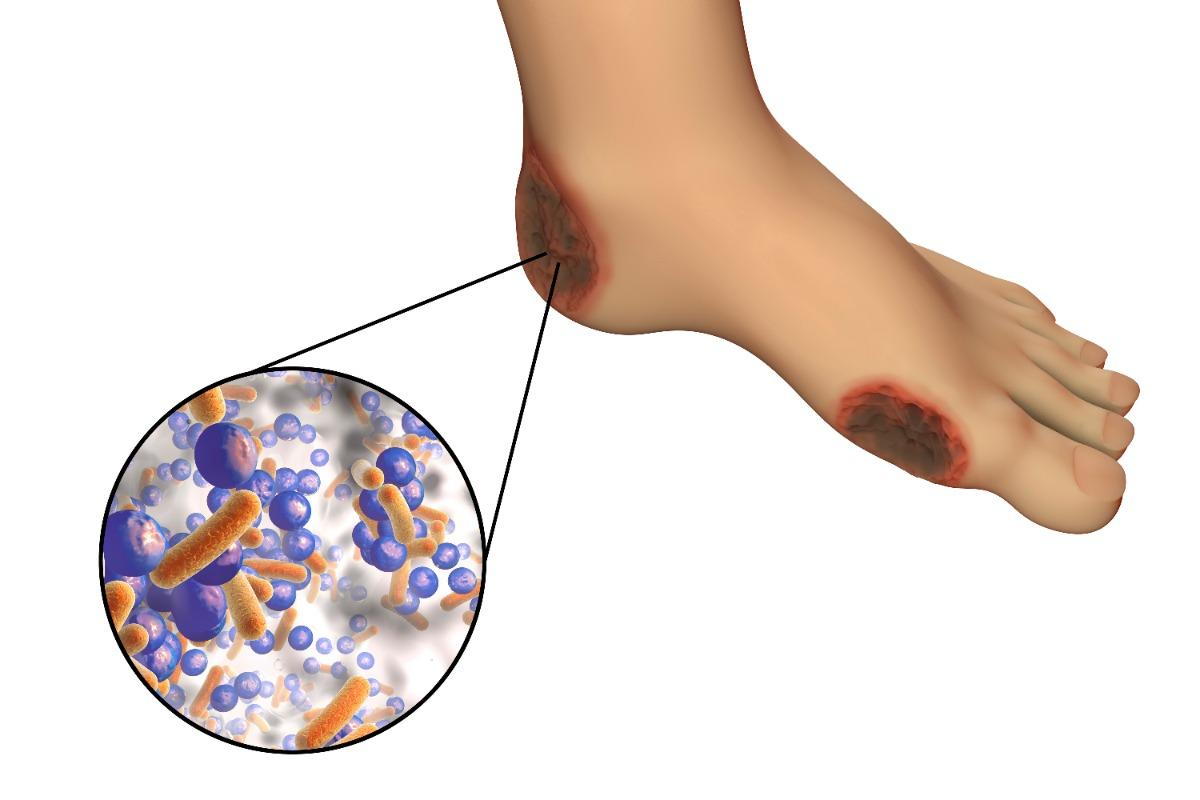
Abscesses
When bacteria enter your body, your immune system sends infection-fighting white blood cells to the affected area. As the white blood cells attack the bacteria, some nearby tissue dies, creating a hole that fills with pus to form an abscess. Pus will appear milky white or yellow and can either be draining from the site or build up underneath the skin. This is often very tender to the touch and typically associated with redness around the site.
Cellulitis
A bacterial infection of the skin. This can present alone or in combination with an abscess, wound, or ingrown nail. The most common bacteria that cause cellulitis are gram-positive organisms, namely Staphylococcus aureus, but they can be caused by many different organisms. People with diabetes often have wounds infected with multiple organisms. Treatment usually includes oral antibiotics as well as treating the underlying cause.
How are skin infections diagnosed?
To diagnose a skin infection, your podiatrist will do a physical exam and ask about your symptoms. Every patient’s case and treatment is unique and thus we will tailor the treatment plan to your specific presentation. We will review your x-rays and, if necessary, order more advanced imaging such as an MRI if the symptoms are more severe to determine if there is an infection in the bone or soft tissues. We often take a culture of the wound or drainage to determine what specific organism is causing the infection in order to determine the best antibiotic. At times we will also order labs (bloodwork) to determine the extent of the infection.
How are skin infections treated?
The treatment depends on the type of infection and how serious it is. Some infections will go away on their own. Oftentimes it will require either topical and/or oral antibiotics and addressing the source of the infection (removing an ingrown nail, draining an abscess, healing the wound, etc)
Patients at increased risk of infections and complications from infections
- Diabetics
- Poor circulation due to PAD (peripheral arterial disease)
- Poor immune system (HIV/AIDS, lupus, etc)
- Immunocompromised (due to medications or chemotherapy)
- Elderly
- Malnourished
- Sedentary patients (those that do not move much due to being hospitalized, elderly, paralyzed, etc)
When to seek treatment
If you notice an abscess you can initially try Epsom salt soaks, warm compresses, a topical antibiotic ointment such as Neosporin, and cover with a bandage. Still, if this doesn’t resolve within a few days you should seek medical attention. You should not try to drain an abscess at home because they lack of sterility can oftentimes lead to further infection.
Symptoms such as nausea, vomiting, fevers, and chills associated with local signs of infection (redness, warmth, drainage, etc) can oftentimes signal that the infection is beginning to worsen and affect the rest of your body. You should either call the clinic for medical advice or if not, present to your local hospital’s emergency department.
If you are a diabetic, immunocompromised, or have poor circulation, you should schedule an appointment with your podiatrist as soon as possible. Infections in these individuals can often worsen quickly and these patients are at an increased risk of poor wound healing.